Unveiling the Hidden Influences on Your Blood Pressure
- Andrew Kowalski
- 7 hours ago
- 7 min read
Andrew Kowalski, MD, FASN
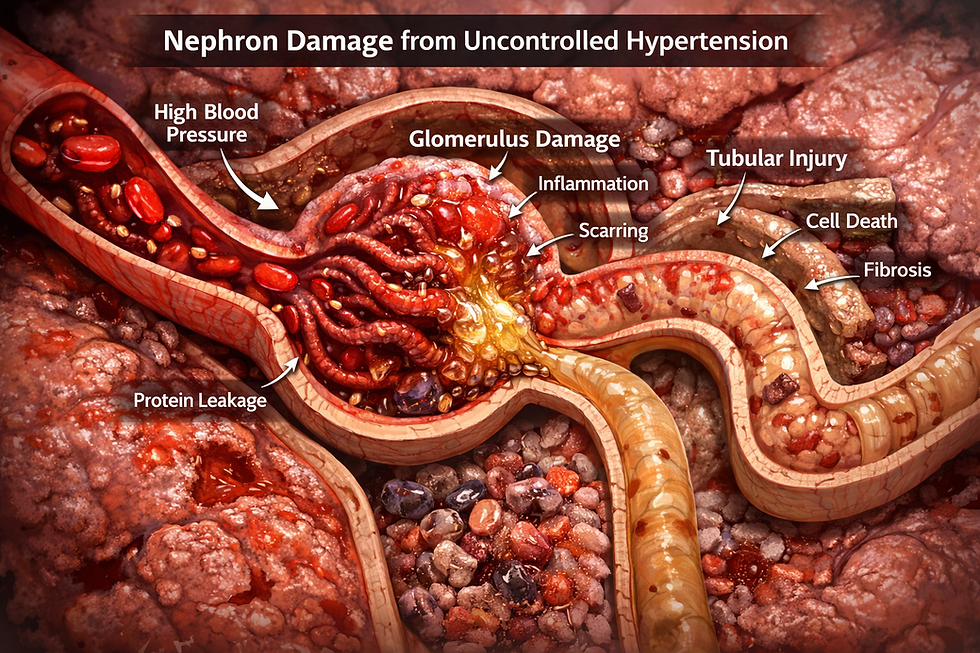
If you're living with kidney disease, you most likely have been told, and likely know that blood pressure control is not just important...it's essential. High blood pressure is both a cause and consequence of kidney damage, creating a vicious cycle that can accelerate disease progression.
But what if I told you that some of the most important factors affecting your blood pressure have nothing to do with the usual suspects like salt intake or stress levels?
Did I just blow your mind?
I’m certain I did...let's dive in!
The long-held Dogma of salt and blood pressure is likely not the whole truth.
Recent scientific discoveries are revolutionizing our understanding of hypertension, revealing surprising connections between blood pressure and everything from the health of your gums to the air quality in your home. For those of us working to protect kidney function, these insights offer powerful new avenues to address and targets to tackle for blood pressure management.
The Scope of the Problem
Let's start with the sobering facts: high blood pressure affects approximately 1.5 billion people worldwide and remains the leading risk factor for premature death globally. For kidney patients, the stakes are even higher. Hypertension damages the delicate filtering units in your kidneys, and conversely, declining kidney function makes blood pressure harder to control.

Here's what concerns me most as a medical educator; about half of the people walking around with high blood pressure don't even know they have it, since hypertension typically causes no symptoms. Even among those with a diagnosis, only one in five has their blood pressure adequately controlled.
Clearly, our traditional approaches aren't enough.
A Paradigm Shift: Your Immune System Is Calling the Shots
For over 70 years, we've viewed high blood pressure through the lens of "pipes and plumbing," focusing on how blood vessels constrict and hearts pump. But groundbreaking research from Professor Tomasz Guzik at the University of Edinburgh has revealed a missing piece of the puzzle: your immune system.
In landmark studies, Guzik demonstrated that mice lacking functional immune systems were protected from developing severe hypertension. When immune cells called T lymphocytes were restored, the mice developed high blood pressure. Subsequent human studies confirmed that the immune system doesn't just participate in hypertension; it can actually cause it.
Here's how it works;
Immune cells infiltrate the walls of blood vessels and organs, releasing inflammatory molecules.
This inflammation stiffens the blood vessels, making blood flow more difficult.
Pressure rises.
Your heart works harder.
Your kidneys retain more salt and water.
A cycle of chronic, low-grade inflammation takes hold throughout your body.
For kidney patients, this inflammatory model of hypertension is particularly relevant, as kidney disease itself is an inflammatory condition that can amplify these processes.
Chronic Inflammation will likely become a major target in controlling and preventing many diseases (ie, CKD, heart disease, stroke, diabetes, etc.) in the very near future.
Your Mouth Matters More Than You Think
One of the most surprising discoveries that came up in the literature involves an unlikely suspect: your gums. Dr. Marta Czesnikiewicz-Guzik, working with genetic data from half a million people in the UK Biobank, demonstrated that severe gum disease (periodontitis) doesn't just occur alongside high blood pressure, it can actually cause it.
The implications became even more exciting when the research team conducted a clinical trial with 100 people who had both hypertension and gum disease. Half received intensive periodontal treatment with deep cleaning below the gumline. The other half received only superficial cleaning above the gumline.
Two months later, the results were clear: those who received intensive gum treatment had not only healthier gums but also lower blood pressure and reduced levels of inflammatory markers in their blood. Inflammation strikes again!

So, schedule that dental cleaning you've been putting off. Floss daily. If you notice bleeding gums or other signs of gum disease, seek treatment promptly. For kidney patients, who already face elevated cardiovascular risk, oral health may be an underappreciated tool for blood pressure control.
The Air You Breathe Could Be Raising Your Pressure
If you live near a busy highway or in a densely populated urban area, traffic pollution may be silently driving your blood pressure upward. Professor Douglas Brugge's research with residents of Somerville, Massachusetts, a city crisscrossed by major highways, revealed that ultrafine particles from vehicle exhaust can trigger systemic inflammation and elevated blood pressure.
In a clever study design, Brugge provided 154 residents living within 200 meters of busy roads with air purifiers. For alternating periods, participants used either genuine high-efficiency particulate air (HEPA) filters or sham devices with the filters removed. When participants with pre-existing hypertension used real air purifiers, their blood pressure dropped by an average of 3 mmHg compared to when they used the sham units.
While 3 mmHg might sound modest, this reduction is clinically meaningful and could help prevent heart attacks and strokes years down the line.
What this means for you: If you live near heavy traffic, consider investing in a HEPA air purifier for your bedroom and main living areas. Keep windows closed during rush hour. While these devices can be expensive, the cardiovascular benefits may make them worthwhile, especially for those with kidney disease who face compounded risks.
Feed Your Gut, Lower Your Pressure
Perhaps the most actionable discovery involves something you can start doing today: eating more fiber. We've long known that high-fiber diets correlate with lower blood pressure and reduced cardiovascular risk, but Professor Francine Marques at Monash University finally explained why.
When gut bacteria digest fiber, they produce molecules called short-chain fatty acids (SCFAs). These compounds interact with immune cells, dialing down inflammatory signals and protecting blood vessels from damage. Essentially, your gut bacteria serve as tiny pharmaceutical factories, manufacturing compounds that help control blood pressure.

Marques put this to the test in a randomized trial with 20 people with untreated hypertension. When participants ate a diet enriched with SCFA-producing fiber (cleverly hidden in burgers, frittatas, and muffins), their blood pressure dropped by approximately 6 mmHg—equivalent to taking one standard antihypertensive medication.
The composition of their gut microbiome shifted too, with an increase in beneficial SCFA-producing bacteria. However, when participants returned to their regular diets, these beneficial bacteria declined, suggesting that fiber intake needs to be a sustained commitment, not a temporary fix.
What this means for you: Aim for at least 25-30 grams of fiber daily from whole food sources like legumes, vegetables, fruits, and if you feel the need whole grains. For kidney patients, work with your healthcare team to identify the best fiber sources that fit within any dietary restrictions you may have (such as potassium or phosphorus limits). Chickpeas, lentils, oats, and many vegetables are excellent choices for most people with kidney disease.
Taking Action: A Comprehensive Approach
The emerging science tells us that blood pressure control requires a multifaceted strategy:
Know your numbers.
Get your blood pressure checked regularly; most pharmacies offer free screenings.
For those with kidney disease, home blood pressure monitoring can provide valuable information between clinic visits.
Don't abandon proven strategies like exercise, weight management, salt reduction, stress management, and adequate sleep. These remain essential.
Embrace the new science.
Prioritize oral health with regular dental care and daily flossing.
If you live near heavy traffic, consider air purification.
Most importantly, make fiber-rich foods a cornerstone of every meal.
Work with your healthcare team. Blood pressure medications remain crucial tools, especially for kidney patients. These new insights complement rather than replace medical treatment.
Think long-term. Whether it's maintaining a high-fiber diet or keeping up with dental cleanings, consistency matters. The benefits accrue over time.
The Bottom Line
The revolution in hypertension research reminds us that human health is interconnected in ways we're only beginning to understand. Your oral health affects your cardiovascular system. The air in your home influences your blood vessels. The bacteria in your gut communicate with your immune system to regulate blood pressure.
For those of us working to preserve kidney function, these discoveries are empowering. While we can't change our genetics or always control our environment, we can take meaningful action today; scheduling a dental appointment, setting up an air purifier, adding an extra serving of fiber-rich foods to our meals.
Blood pressure control isn't just about numbers on a monitor. It's about protecting your kidneys, your heart, and your future. With these new insights, we have more tools than ever to do exactly that.
Remember: Always consult with your nephrologist or healthcare provider before making significant changes to your diet or treatment plan, especially if you have kidney disease with specific dietary restrictions.
References and Further Reading
Guzik TJ, Hoch NE, Brown KA, et al. Role of the T cell in the genesis of angiotensin II induced hypertension and vascular dysfunction. Journal of Experimental Medicine. 2007;204(10):2449-2460.
Czesnikiewicz-Guzik M, Lee WW, Cui D, et al. T cell subset-specific susceptibility to aging. Clinical Immunology. 2008;127(1):107-118.
Muñoz Aguilera E, Suvan J, Buti J, et al. Periodontitis is associated with hypertension: a systematic review and meta-analysis. Cardiovascular Research. 2020;116(1):28-39.
Czesnikiewicz-Guzik M, Osmenda G, Siedlinski M, et al. Causal association between periodontitis and hypertension: evidence from Mendelian randomization and a randomized controlled trial of non-surgical periodontal therapy. European Heart Journal. 2019;40(42):3459-3470.
Brugge D, Durant JL, Rioux C. Near-highway pollutants in motor vehicle exhaust: A review of epidemiologic evidence of cardiac and pulmonary health risks. Environmental Health. 2007;6:23.
Allen RW, Barn P, Lanphear BP. Randomized controlled trials in environmental health research: unethical or underutilized? PLoS Medicine. 2009;6(1):e1000016.
Marques FZ, Nelson E, Chu PY, et al. High-Fiber Diet and Acetate Supplementation Change the Gut Microbiota and Prevent the Development of Hypertension and Heart Failure in Hypertensive Mice. Circulation. 2017;135(10):964-977.
Marques FZ, Mackay CR, Kaye DM. Beyond gut feelings: how the gut microbiota regulates blood pressure. Nature Reviews Cardiology. 2018;15(1):20-32.
Verhaar BJH, Prodan A, Nieuwdorp M, Muller M. Gut Microbiota in Hypertension and Atherosclerosis: A Review. Nutrients. 2020;12(10):2982.
Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nature Reviews Nephrology. 2020;16(4):223-237.
World Health Organization. Hypertension. Available at: https://www.who.int/news-room/fact-sheets/detail/hypertension (Accessed 2024).
Guzik TJ, Touyz RM. Oxidative Stress, Inflammation, and Vascular Aging in Hypertension. Hypertension. 2017;70(4):660-667.



Comments