Understanding the Link Between Metabolic Acidosis and Chronic Kidney Disease
- Andrew Kowalski
- Nov 28, 2024
- 6 min read
Andrew Kowalski, MD, FASN
Chronic kidney disease (CKD) is a long-term condition in which the kidneys gradually lose their ability to filter waste, balance electrolytes, and maintain fluid homeostasis. One of the lesser-known yet significant complications that can arise in people with CKD is metabolic acidosis. Understanding the relationship between metabolic acidosis and CKD is crucial for both patients and healthcare providers, as proper management can slow down the progression of kidney disease and improve overall quality of life. The goal is to aim for a serum bicarbonate level to be above 22mEq in CKD patients.
What is Metabolic Acidosis?
Metabolic acidosis occurs when the body produces too much acid or when the kidneys are unable to remove enough acid from the blood.
So where does this acid come from?
Healthy kidneys maintain acid balance by excreting it in the urine. Acidosis is caused by an accumulation of these acids in the blood and other body fluids, which typically occurs when kidney function falls below 45%.
In a healthy individual, the kidneys and lungs work together to maintain a balanced pH, which is typically between 7.35 and 7.45. However, when the kidneys are impaired, they struggle to eliminate hydrogen ions (acid) and may also fail to reabsorb bicarbonate, a base that helps neutralize acid. This imbalance leads to a
buildup of acid in the bloodstream, known as metabolic acidosis.

Some additional causes of acidosis in the body
How Does CKD Cause Metabolic Acidosis?
As CKD progresses, the kidneys lose their ability to perform essential functions, including acid-base balance. Normally, the kidneys excrete acids generated from metabolism, particularly from the breakdown of dietary proteins. However, in CKD, this process becomes compromised. The kidneys are less efficient in excreting acid, and bicarbonate levels in the blood decrease. This results in a condition known as chronic metabolic acidosis, which is common in the later stages of CKD.
The body tries to compensate for the acid buildup in various ways, including:
1. Bone buffering: The body draws on bone minerals, like calcium and phosphate, to neutralize excess acid. Over time, this can lead to bone weakness and increase the risk of fractures.
2. Muscle breakdown: Protein breakdown can occur in an attempt to use the released amino acids as buffers. This process contributes to muscle wasting, a condition frequently observed in people with advanced CKD. Muscle wasting can also contribute to worsening kidney function as will be explaied inn a later post.
3. Respiratory compensation: The lungs may try to expel more carbon dioxide (which is acidic) through faster or deeper breathing, but this is often insufficient to fully correct the imbalance.
Why Is Metabolic Acidosis a Problem in CKD?
Metabolic acidosis can have serious consequences for people with CKD, accelerating the decline in kidney function and affecting overall health. Some of the key impacts include:

1. Worsening of Kidney Function: Metabolic acidosis can further damage kidney cells, worsening CKD progression. Studies suggest that acidosis promotes inflammation and fibrosis (scarring) in the kidneys, which can lead to a faster decline in kidney function.
2. Bone Health: As mentioned earlier, the body uses calcium from bones to buffer excess acid. Over time, this depletes bone minerals, increasing the risk of osteoporosis and fractures. CKD patients with untreated metabolic acidosis are at a higher risk for bone diseases like renal osteodystrophy.
3. Muscle Wasting: The body’s attempts to neutralize acid by breaking down muscle tissue lead to muscle weakness and wasting, which can affect mobility and overall physical health.
4. Cardiovascular Risk: Acidosis can impair heart function and increase the risk of cardiovascular diseases. CKD patients are already at a higher risk of heart disease, and metabolic acidosis further elevates this risk by causing changes in blood pressure and vascular health.

How is Metabolic Acidosis Diagnosed and Treated in CKD?
Metabolic acidosis is usually diagnosed through blood tests that measure serum bicarbonate levelsand the blood pH. A bicarbonate level below 22 mEq/L or a blood pH below 7.35 may indicate metabolic acidosis.
In people with CKD, treating metabolic acidosis is critical to slow down the progression of the disease and prevent complications. The main treatments include:
1. Dietary Changes: Reducing the intake of animal proteins, which produce more acid, can help manage acidosis. Plant-based proteins are often recommended, as they produce fewer acidic byproducts. Although this topic is under some debate and there is still no concrete consensus. Newer methods of management do allow for people with CKD to continue to consume animal products, but the bottom line is that plant based protein do contribute less to the overall acid load and a full amino acid profile can be obtained through a plant based diet (although it does take some throught and planning).
2. Bicarbonate Supplementation: Sodium bicarbonate (baking soda) or other alkalinizing agents are commonly prescribed to raise bicarbonate levels and correct acidosis. Studies have shown that bicarbonate supplementation in CKD patients can slow down kidney function decline and improve muscle mass. The goal is to achieve a serum bicarbonate level above 22mEq and ideally above 24 to achieve the benefits of correcting acidosis and there are numerous studies that show a slowing in CKD progression just by elevated the serum bicarbonate level. For reference that is equivalent to adding 3 cups of fruits and/or vegetables to your diet each day...very doable.
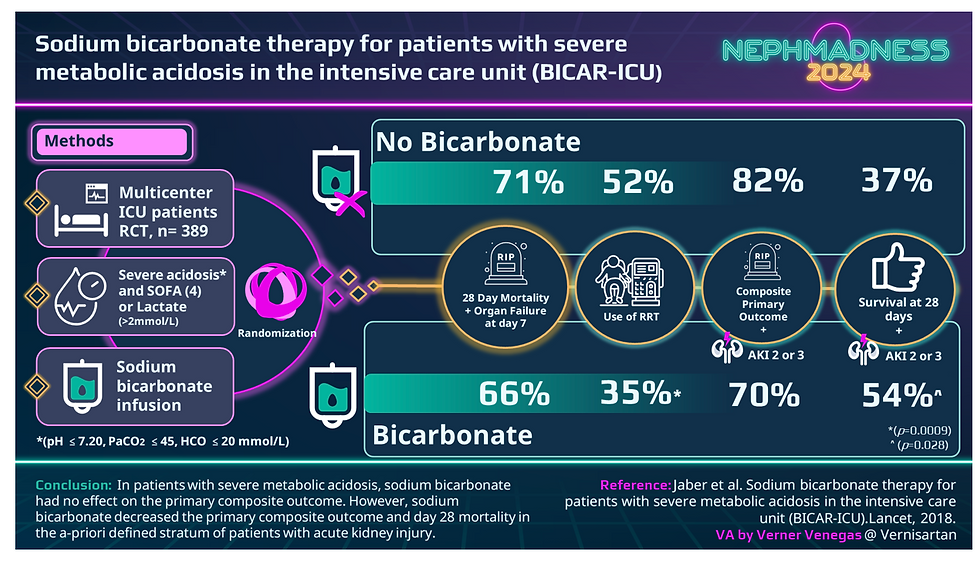
The BICAR-ICU study was looking at correcting bicarbonate in the ICU setting. Unfortunately, the need to control acid is not the only problem in severely sick patients in the ICU. This can lead to some confusion among patients who will see this and say that giving bicarbonate does not improve mortality, but it does when addressing the other components in these very sick patients.
The study aimed to determine if administering sodium bicarbonate would enhance the pre-specified primary outcome of 28-day survival compared to the control group receiving usual care. Although the treatment group maintained a higher pH, there was no difference in the primary outcome between the two groups.
Many of the issues reported were related to how the bicarbonate was given. If given with IV fluid the patient can easily become overloaded leading to a slew of new complications. However, patients with AKI showed a mortality benefit and a decreased need for dialysis, even though the study was not designed for subgroup analysis.
3. Managing Protein Intake: While reducing dietary protein can help reduce acid load, it’s essential to balance this with the body’s nutritional needs, especially in patients who may already be suffering from muscle wasting. The pendulum is finally swining in the other direction sugesting that limitting protein intake is a short term answer and will make your blood number look better in the short term. Now we are recognizing that even though the short term benefits are comforting to the healthcare provider, the long term effects become more concerning and harder to manage,
4. Pharmacological Treatments: In some cases, medications that help buffer acid or reduce acid production may be prescribed. These medications can be especially useful in more advanced CKD when dietary adjustments and bicarbonate supplements alone are insufficient. Although other medications are around, I have yet to have bicarbonate supplementation fail. In a recent study called VALOR-CKD, using a hydrogen binging medication did not slow CKD damage. What was not talked about in the study is that other bicarbonate studies aimed to raise the serum bicarbonate levels much higher than 22mEq and those showed benefit. Clinitions need to be more aggressive and the goal will be achieved. Also adding more fruits and vegetables as mentionsed above will help significantly.

The Bottom Line
Metabolic acidosis is a common and serious complication of chronic kidney disease that can accelerate the progression of CKD, worsen bone and muscle health, and increase cardiovascular risks. Early diagnosis and appropriate management, including dietary changes and bicarbonate supplementation, are critical to mitigate its effects. By addressing metabolic acidosis, healthcare providers can help CKD patients maintain a better quality of life and potentially slow down the progression of kidney disease.
If you or a loved one has CKD, it’s essential to discuss metabolic acidosis with your healthcare provider to ensure that it is properly managed. Regular monitoring of kidney function and blood acid levels, alongside proactive treatment, can make a significant difference in long-term outcomes.




Comments